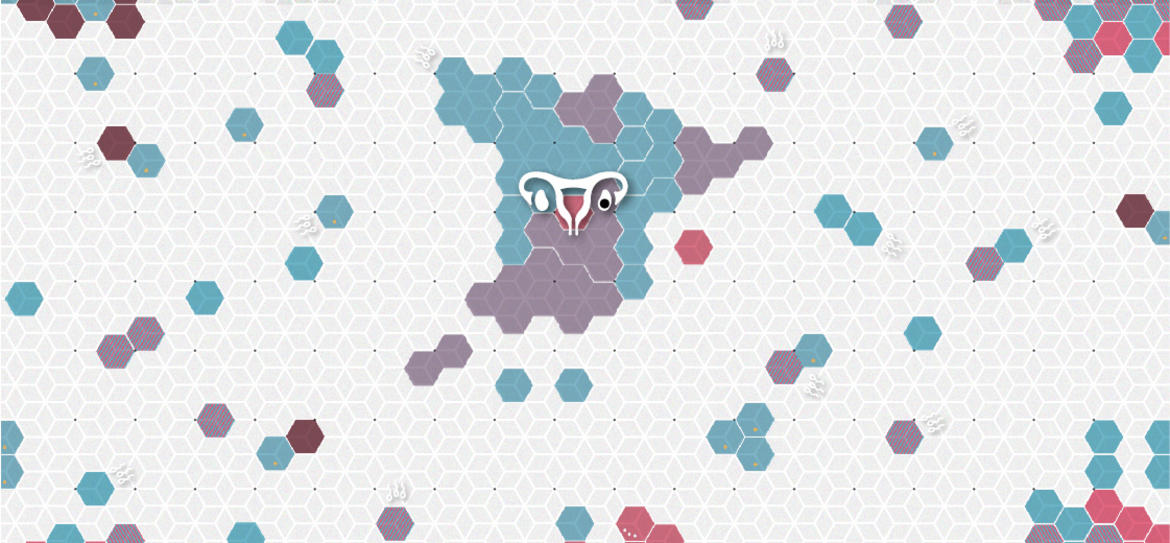
The postcode lottery of publicly-funded assisted reproduction in Spain
Many autonomous communities are not providing the bare minimum of provision in Spain’s health service and are using stripped back services, age limits and imposing fees in order to avoid providing the service.
None
The postcode lottery of publicly-funded assisted reproduction in Spain
Many autonomous communities are not providing the bare minimum of provision in Spain’s health service and are using stripped back services, age limits and imposing fees in order to avoid providing the service.
For women like Izaskun Gamen, the decision taken only a week ago to include single women, same-sex couples and trans people capable of pregnancy among those eligible for publicly-funded assisted reproduction “is very welcome because it’s been a long time coming”. Although she is pleased for those who will receive treatment in the future, she cannot help but look back and remember that, for years, she was unable to access in vitro fertilization on account of her single status.
In 2014, the Partido Popular government excluded single women from assisted reproduction services on the national health service. Little by little, however, most autonomous communities modified their laws to offer them treatment. Almost all were offering it to single women. But there were a few exceptions: Ceuta and Melilla did not have the appropriate services available, while Navarra offered single women the option of artificial insemination (cheaper yet less effective than in vitro). It was in vitro that Izaskun Gamen needed. The activist, a member of Madres Solteras por Eleccion (MSPE, Single Mothers by Choice), lives in Navarra. For years, she fought against this discrimination. “The injustice of ‘yes to them, no to others’ hurt me deeply. It made me depressed”, she says. It provided a further injustice to women suffering from illnesses such as endometriosis , which greatly limits the possibility of pregnancy without in vitro fertilisation, as described in the case brought to the ombudsman in Navarre in 2019.
The measure has now been approved, but was announced in 2018 and it never came to pass. “It’s now possible, but no one remembers the bad times” she laments. That is because, as she turns forty in January (the age limit for publicly accessing in vitro fertilization), the decision has been made too late. Along the way, she wasted €20,000 made from second jobs in three years of attempts through private healthcare, on top of numerous attempts at artificial insemination, an inadequate technique – though the only one she could access through the state.
Now she finds herself in Valencia, far from Tudela, where she lives, giving it one last go at becoming a mother. She laments the fact that the government only found out about their organisation – which had been campaigning for years – through the press. She also points out that another form of discrimination that was present in the previous law has not been changed: public healthcare does not cover in vitro fertilisation for mothers or couples who already have a healthy child. This means that a single woman who has had a child with a previous partner cannot access this treatment, but can if she attempts treatment with a new partner.
With its latest decision, the Government has levelled the playing field for women’s access to publicly-funded in vitro fertilisation. As there is only a law of minimum provision across the country, though, some autonomous communities implement it restrictively, imposing age limits, a maximum number of attempts, and restrictions on the physical state that a woman must be in in order to receive treatment.
The thousands of ways to interpret an age limit
Given that in Spain the average age of maternity has risen over the past decade from 29.82 to 31.22 years, more and more women are finding themselves wanting to conceive above the age of 35. National law now states that the age limit to undergo this treatment is 40 for women and 55 for men. Specifically, the woman cannot be past her fortieth birthday “at the start of the patient’s consultation”. This age limit drops to 38 in the case of insemination with a partner’s semen.
However, what does “the start of the consultation” mean? Although the logical interpretation would seem to suggest the first appointment, meaning that women could pass the age limit during their treatment as long as they had had an appointment before their fortieth birthday, some autonomous communities twist this interpretation of the law and end up denying women their treatment prematurely. In Madrid and the Basque Country , for example, if one turns 40 between treatment cycles, the treatment is ended. This is an incredibly restrictive interpretation of state law: each “consultation” is determined to begin at the start of each treatment cycle, rather than just at the beginning of the whole treatment process.
Last April, the Galician ombudsman published a resolution urging a hospital to continue treatment – which had been interrupted in contravention of national protocol – for a woman who had turned 40 between her first and second artificial insemination cycles.
As above-mentioned, the age limit of 40 is lowered to 38 for insemination by a partner, though only in this instance, according to state law. However, there are some communities that have manipulated this measure as well: the Balearics and Catalonia have both imposed this age limit for insemination by donor semen, even though Spanish law is clear that the age limit for this kind of treatment is 40.
The age limit is crucial, considering that the waiting lists can make someone wait years to access a treatment. Given that the law only takes into account age, rather than medical context, many women are refused the opportunity to become mothers on account of delays in the health service. For example, if a thirty-eight-year-old woman is registered on the waiting list and has to wait three years, she will be ineligible at the start of treatment. In the Canaries , if officials find that you will turn 40 on the waiting list, you are automatically excluded.
From the little data available regarding the waiting time for assisted reproduction, after El País gained access to an internal audit, one can see that in Madrid, in 2018, three public hospitals had a wait of more than one year to access assisted reproduction. This is nothing however, compared to the three years wait for treatment at the Hospital Clínico San Carlos, also in Madrid. In the Hospital Universitario Cruces in Barakaldo, the average wait time between registration on the waiting list and in vitro fertilisation is nine months, according to their own web page . We also know that, on 31st December 2020, Castilla y León had around fifty people on its waiting list for an initial consultation for assisted reproduction at the Hospital Universitario Rio Hortega in Valladolid, and a dozen waiting at the Hospital Clínico Universitario de Valladolid. These are the only two hospitals in the autonomous community that carry out in vitro fertilisation, and so, no matter which part of Castilla y Leon you live in, you have to move to Valladolid if you would like to publicly access the treatment and get on the list.
A fall in the number of attempts
Even when age is not a problem, there are other barriers that can exclude women from publicly funded treatment. The most relevant is a cap on the number of attempts that the state is willing to cover. The vast majority of autonomous communities follow the national lead in setting the cap at three attempts, apart from the slightly more generous La Rioja, which allows four. Then there is Catalonia , which ignores national minimums and only allow two attempts for donated sperm (although the limit can rise to three attempts if the woman is under 35).
Regarding artificial insemination, six attempts with donor semen and four with a partner’s semen are generally permitted. Given that it is a less effective method, one can understand that most women turn to in vitro before exhausting all their attempts, though in this case, one should be allowed to use up all attempts allowed by the state minimum. This is where the compliance of autonomous communities differs wildly.
State law dictates that the number of attempts “can be reduced according to prognosis and the number of previous attempts”. This is the case in the Basque Country, that includes all previous attempts, both at public and private clinics, to add up to three attempts. This means that, were you to be previously treated at a private clinic, paying from your own pocket, you would have fewer publicly funded attempts.
More barriers and more failures
The physical condition of the person undergoing treatment, the number of children that they already have, or copayment for medicine or semen, are other barriers to accessing publicly-funded assisted reproduction. State law excludes those who already have healthy children from accessing treatment, including partners, as well as those who have had voluntary sterilisation, or in cases in which treatment could pose a serious risk to the health of the mother or child. This interpretation changes from community to community.
In Andalucía and Asturias , for example, drug users are excluded from treatment. In the Basque Country , La Rioja and Andalucía , treatment is not given to women with HIV or hepatitis, for fear of spreading the diseases.
Eleven autonomous communities impose weight restrictions. Andalucía is the most strict, with a BMI requirement range between 19 and 30. The argument is that, according to protocol, going above or below this range “lowers the possibility of conception” and a healthy weight reduces risks during pregnancy.
Treatment would be denied, for example, for being too thin to a woman who is 1.6m tall and weighs 45 kilos (BMI of 17.58) in Aragon, Cantabria, Murcia, Asturias or Andalucía . If this same woman weighs 85 kilos (BMI of 31.22) she will be refused treatment in Andalucía , Asturias , Extremadura and La Rioja for having too high a weight. According to Spain’s National Statistics Institute (INE), between 13% and 14% of women between 35 and 44 would not fall within the weight limits imposed by law.
Furthermore, in Andalucía , Asturias , Castilla La Mancha and Murcia, a woman cannot access treatment if she has frozen embryos. The same applies in Aragón and Extremadura , and these communities also deny access to women who have cryogenically frozen their eggs.
However, even when publicly funded, the cost for the woman receiving fertilisation treatment is not nothing. For example, there is copayment for medication, although the cost is much smaller than it is in a private clinic.
In some communities, there is an extra charge: if you need donated sperm in Madrid , it must be paid from your own pocket to a private bank with which the clinic has an agreement. This exists in La Rioja with similar charges for eggs. The Community of Madrid claims that there are not enough public sperm banks, even though there are seven registered in the community. The other autonomous communities cover these costs, even if they have to buy sperm from external laboratories.
All these barriers, regardless of where one lives, exclude women from publicly funded assisted reproduction, and at what cost. Treatment in private clinic is wildly expensive: a single treatment cycle for artificial insemination, with the semen of a partner, can range between €385 and €1,200, while in vitro fertilisation can cost between €2,650 and €4,995. All this is multiplied by the number of attempts, without taking into account extra medication and tests.
Methodology
We carried out a search of the assisted reproduction protocols for every autonomous community. Therefore, we were able to compare information from Andalucía , Asturias , the Canaries , Castilla La Mancha , Catalonia , Extremadura , Madrid and the Basque Country . Furthermore, in the case of Aragón, Asturias, the Balearics, Cantabria, Castilla-La Mancha, Castilla y León, Catalonia, Valencia, Extremadura, Galicia, La Rioja, Madrid, Murcia, Navarra and the Basque Country, we received information through the press office of the Department of Health. Nevertheless, upon finishing this article, the Canary Islands had not got back to us on the number of partner-provided fertilisation cycles covered by the state; Nor had Catalonia responded to our request for an updated version of their assisted reproduction protocols (the most current version is from 2016). The Asturian Department of Health did not confirm its policy on treatment for single women before the approval of the new laws, though we managed to access the information thanks to Dr. Ángel Plácido Llaneza Coto , Director of the Human Assisted Reproduction Unit at the Hospital Universitario Central de Asturias. For their part, Ceuta and Melilla depend on the Spanish Government’s Ministry of Health, as they apply the basic criteria of the national law.
To provide prices of private clinics, we consulted the webpages of ten different private clinics in Spain (Dexeus, Clínica Fertia, IVI, Eva Fertility Clinics, Love Fertility Clinic, Arpa Médica, Institut Marquès, Ginefiv, Easyfiv y Eugin), taking into account artificial insemination via a partner and in vitro fertilisation through one’s own gametes, without any further treatment.
You can find all the data here .
